Coenzyme Q10
Coenzyme Q10 is a fat-soluble substance produced by the liver. Some amount of Q10 is obtained from a diet. In terms of its properties CoQ10 resembles vitamins. Coenzyme Q10 is involved in production of energy and is also an important antioxidant. Many neurodegenerative disorders are related to low levels of this substance.
Coenzyme Q10 (CoQ10) is a naturally occurring component in living cells. It physiologically acts as a powerful antioxidant, membrane stabilizer and cofactor in the production of adenosine triphosphate (ATP) by oxidative phosphorylation, inhibiting the oxidation of proteins and DNA. ATP is a nucleotide with a very important role in the metabolism of living organisms. It is a universal source of energy for biochemical processes in organisms. Accordingly, CoQ10 is important for both metabolic and biochemical processes in the body.
CoQ10 was first approved in 1973 in Japan as a drug for the treatment of patients with heart failure, and it has been used as a drug in some other countries as well. However, in most countries such as the United States and the Europe, CoQ10 has been widely used as a food additive or dietary supplement for maintaining healthy body condition for more than 20 years .
CoQ10 or ubikuinone was known to play a key role in mitochondrial bioenergetics as a carrier of electrons and protons. Subsequent studies showed the presence of CoQ10 in other cell membranes and blood plasma, and its antioxidant role was extensively studied. In addition, recent data suggest that CoQ10 affects the expression of genes involved in the signaling, metabolism and transport of human cells. CoQ10 deficiency is associated with autosomal recessive mutations, mitochondrial diseases, aging-related oxidative stress and carcinogenesis processes, and secondary effects of statin (lipid-lowering drug class). Many neurodegenerative disorders are associated with low levels of CoQ10: diabetes, cancer, fibromyalgia, muscular and cardiovascular diseases.
While many people’s bodies make all the CoQ10 they need, some don’t. The body contains between 500 and 1,500 milligrams of CoQ10, and it decreases with age.
There are no known ideal dosages, as they vary from person to person. Standard dosages for CoQ10 supplements range between 60 and 500 milligrams daily, and the highest recommended daily allowance is around 1,200 milligrams. Possible causes of CoQ10 deficiency:
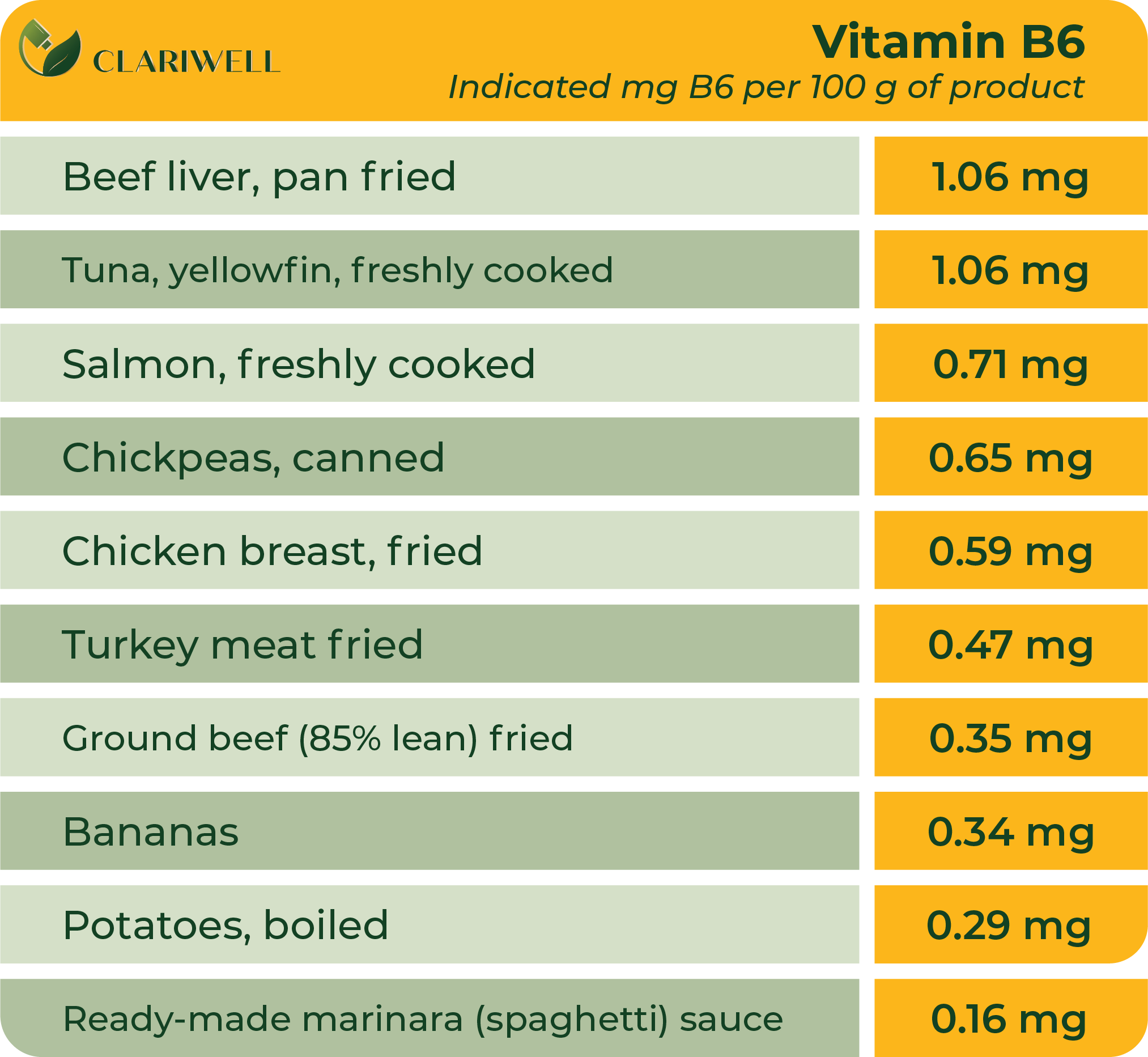
- Deficiencies of certain vitamins, such as vitamin B6
- Mitochondrial diseases
- Genetic defects affecting CoQ10 production
- Oxidative stress, or an imbalance of free radicals and antioxidants
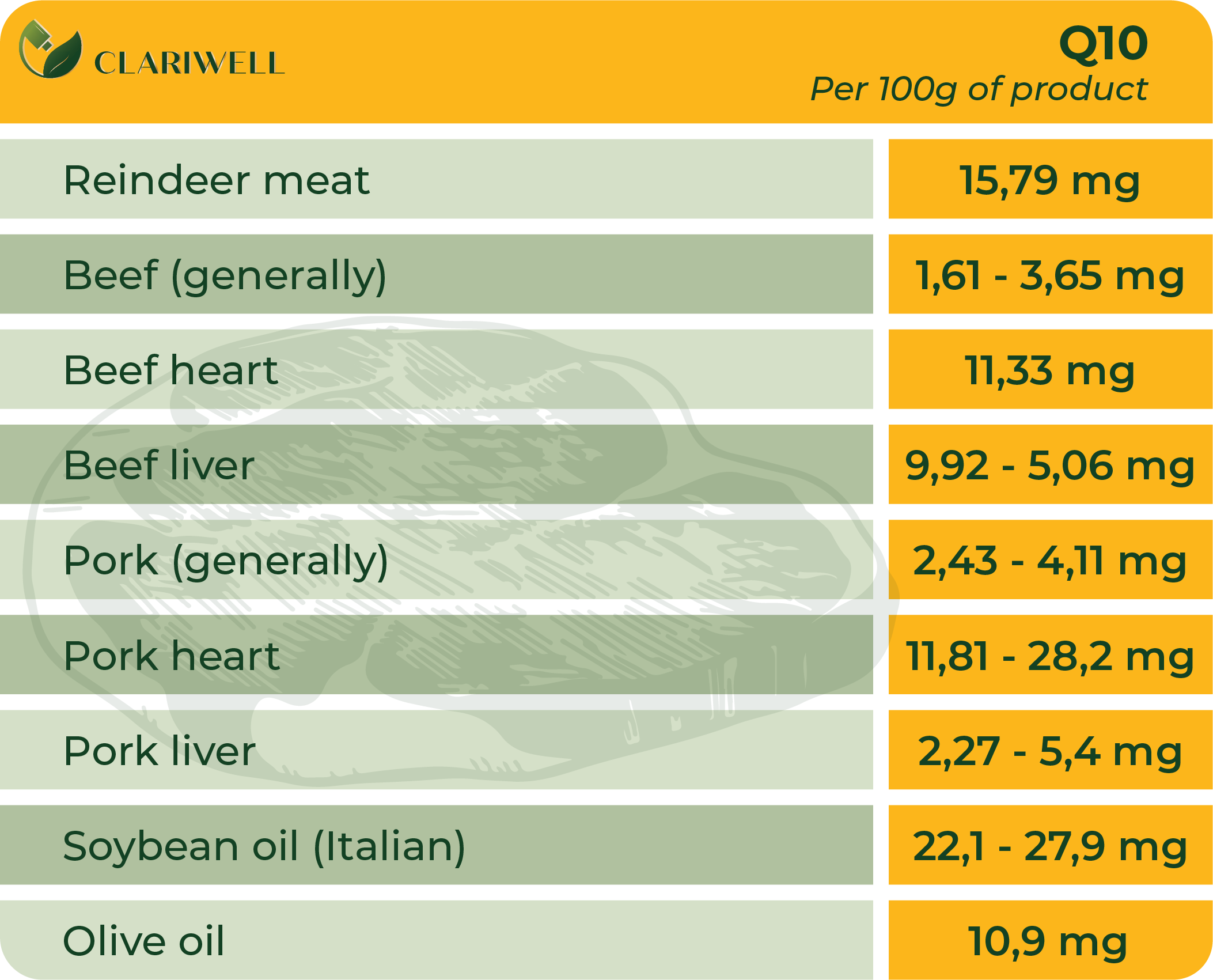
Some CoQ10 containing foods include:
- Organ meats (heart, liver and kidney) contain the highest amounts of CoQ10 per 100 grams.
- Fatty fish, like trout, mackerel, and sardines contain CoQ10.
- Meat
- Soybean products such as tofu, soy milk, and soy yogurt are a valuable source of protein as well as CoQ10 for people who do not eat meat.
- In addition to many vitamins and minerals, a lot of vegetables and fruits contain CoQ10. Notably, broccoli, spinach, avocados and blackcurrants.
Adults who are not found or established to be deficient in CoQ10 are normally required 90- 200mg of CoQ10 per day.
CoQ10 has been used as a dietary supplement or a drug for more than 30 years. Published data of pre-clinical and clinical safety studies have shown that CoQ10 does not cause serious adverse effects in humans, and it is safe for use as a dietary supplement. Pharmacokinetic studies in animals and humans suggest that exogenous CoQ10 does not influence biosynthesis of CoQ nor does it accumulate into plasma or tissues after cessation of supplementation.
Coenzyme Q10 (CoQ10) is one of the most powerful antioxidants in the body, which also restores other antioxidants in the body and plays an important role in protecting against damage caused by reactive oxygen (reactive oxygen can destroy human cells). CoQ10 is the only known lipid-soluble antioxidant! During chronic migraine, inflammatory processes are formed that interfere with replenishment of antioxidant stores, thus reducing the possibility of getting rid of migraine discomfort.
CoQ10 is mainly found in the mitochondria of cells and it helps to improve cellular functions thus reducing the inflammation during a migraine. Since migraine and inflammation are interrelated, CoQ10 could mitigate or even prevent migraine-induced headache.
The pathophysiology of the migraine is not fully understood yet, however blood vessel and neuron dysfunction may be explained with oxygen exchange problems which stem from mitochondrial dysfunction. When it comes to problems with mitochondria, at least some part of patients and, taking into account the important role CoQ10 has to play in accumulating mitochondrial energy, CoQ10 could become a good substance for migraine prevention.
- Fat-soluble, vitamin-like substance that occurs primarily in the mitochondria of practically every cell in the body.
- It is responsible for generating 95 percent of the human body’s energy.
- Both natural and synthetic form of CoQ10 is available; ubiquinone is produced through a proprietary bacteria-production process; ubiquinol is manufactured via yeast fermentation.
- The heart is a remarkable organ as it beats 100,000 times every 24 hours and 2.5 billion times by the age 70, without a single holiday. Consequently, it requires a huge amount of energy. For this reason, nature has placed more CoQ10 in the heart than any other organ.
- There is a belief, that 50% of overweight patients have low levels of CoQ10. Speeding up metabolism with CoQ10 is a safe way to help in weight loss.
- Several studies have concluded that supplementing with CoQ10 may improve sperm quality, activity and concentration by increasing antioxidant protection

Vitamin B2 or Riboflavin
Riboflavin is a water-soluble vitamin, a part of ferment systems which are involved in cellular respiration, carbohydrate and protein breakdown. It is required for optimum functioning of the gastrointestinal tract, blood cells and brain. The main lines of research into riboflavin are related to its impact on tumours and migraine headaches.
Riboflavin was discovered by Blyth in 1872 as a yellow fluorescent pigment in milk, but the vitamin property of this pigment was not established until the early 1930s. Plants and some micro-organisms can synthesize riboflavin; however, it is an essential nutrient for human health and should be obtained from the diet.
Riboflavin, vitamin B2, is a thermally stable, water-soluble vitamin used by the body to metabolize carbohydrates, fats, and protein into glucose for energy. In addition to boosting energy levels, this vitamin functions as an antioxidant for the proper functioning of the immune system, healthy skin, and hair. These effects occur with the help of two coenzymes, flavin mononucleotide (FMN) and flavin adenine dinucleotide (FAD). In riboflavin deficiency, macronutrients like fats, carbohydrates, and proteins cannot be digested to properly maintain the body. Riboflavin is required for normal development, lactation, physical performance, and reproduction.
A healthy digestive system can absorb most of the nutrients from the diet, so it is important to get most of the riboflavin from dietary sources. As already mentioned, Riboflavin has a yellow-green, fluorescent pigment, which causes urine to turn yellow, indicating that the body is absorbing riboflavin. Riboflavin also helps convert tryptophan to niacin, which activates vitamin B6.
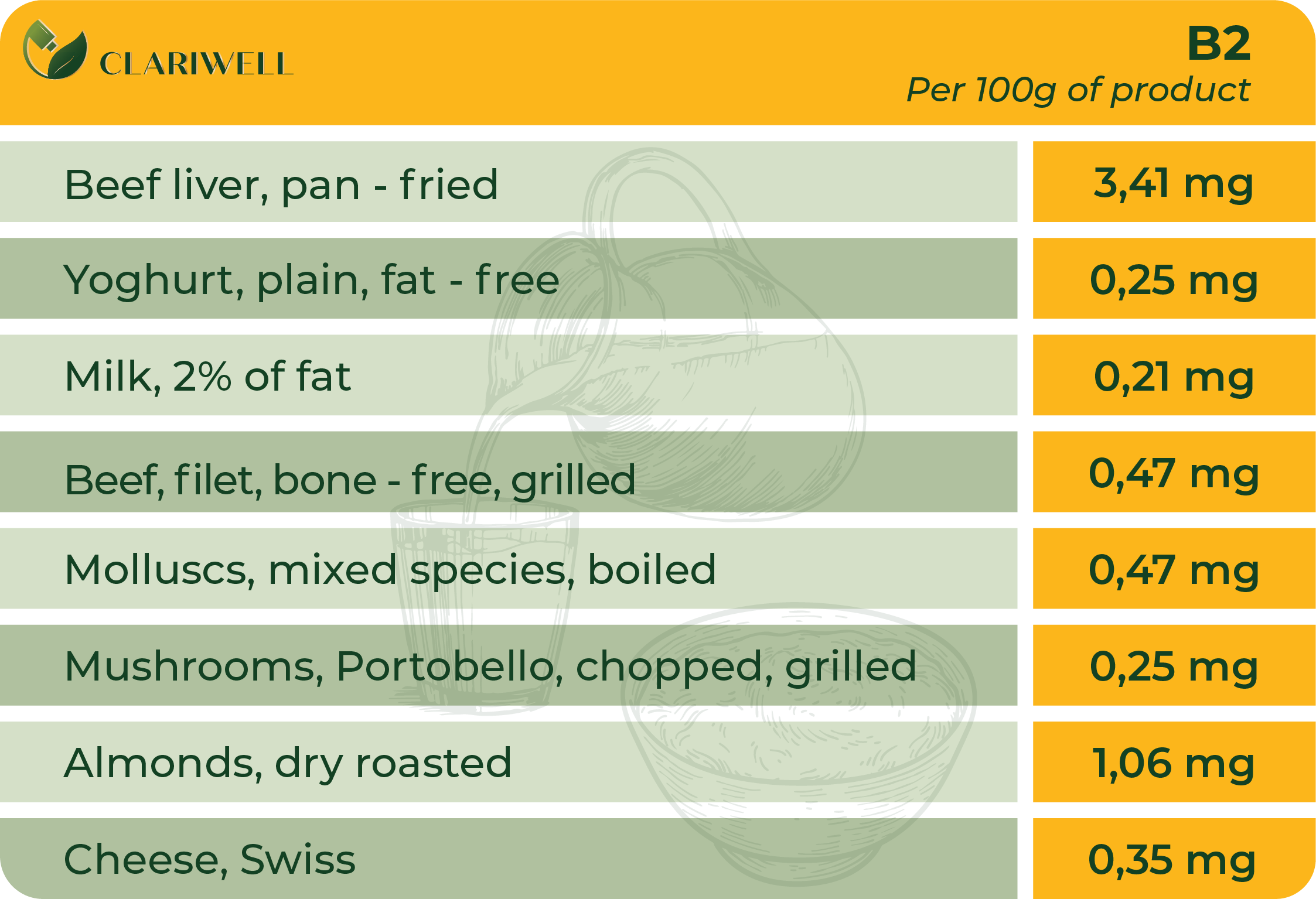
Riboflavin deficiency can be caused by insufficient intake of nutrients or pathologies of the endocrine system. Riboflavin deficiency interacts also with deficiency of other B group vitamins. It is naturally occurring in food products such as eggs, dairy products, meat, green vegetables and grains. Antioxidant riboflavin has the same pathway as glutathione. Glutathione is a natural antioxidant created in our bodies, a simple peptide consisting of three amino acids – glycine, cysteine and glutamine. It possesses several vital properties that regulate bodily processes – immunity boosting, energy production, slowing down of cell ageing, lowering cholesterol level. All cells of the body synthesize glutathione but on a daily basis it can be inhibited and reduced by a number of factors, such as poor nutrition, use of drugs, stress, infections. Glutathione aims at neutralising free radicals and liver detoxification because free radicals can contribute to development of several diseases. A reason of deficient riboflavin can be also chronic diarrhoea, liver problems, alcoholism and haemodialysis.
Groups at risk of riboflavin deficiency are:
Athletes. Exercise load strains metabolism therefore riboflavin is consumed excessively.
Pregnant and breastfeeding woman (sometimes also infants). Pregnant or lactating women who rarely consume meats or dairy products are at riboflavin deficiency risk, which can have adverse effects on the health of both mothers and their infants. Riboflavin deficiency during pregnancy, for example, can elevate the risk of preeclampsia.
Vegetarians or vegans and/or persons who consume very little of milk. Those who eat meat and dairy products obtain a substantial proportion of riboflavin from their diets. For this reason, people who live in developing countries and have limited intake of meat and dairy products are exposed to increased riboflavin deficiency risk. Vegans and those who consume little milk in developed countries are also at riboflavin inadequacy risk.
Adults who are not found or established to be deficient in Vitamin B2 are normally required 1.3 mg for men, 1.1 mg for women and 1.4 mg for pregnant women of Vitamin B2 per day.
When supplementing with riboflavin, appropriate amount is five to ten times the daily recommended allowance (1.3 mg for men, 1.1 mg for women and 1.4 mg during pregnancy). No toxic or adverse effects from intake of high riboflavin doses by humans have been reported so far. However, it can be suggested that a high dose of riboflavin could cause an imbalance in the antioxidant state of human body. However, there is no strong evidence in this area, calling for further investigations to clarify the possible adverse effects of high riboflavin intake.
Allergic reaction to this vitamin is rare. However, seek medical help right away if you notice any symptoms of a serious allergic reaction, including rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, troubled breathing. However, this is not a complete list of possible side effects.
Migraine headache usually presents as intense pulsating or stabbing pain in one area of head. Sometimes it is accompanied by aura (transient focal neurological symptoms before or during headache). In case of some types of migraine there is an established causality of mitochondrial dysfunction. Since riboflavin is required for mitochondria to function, researchers are looking at riboflavin as a possible remedy for preventing or treating migraine headache.
Several studies have been carried out involving riboflavin as migraine prevention or treatment agent. Some of these studies chose large doses of riboflavin – 400mg and more per day, yet several research have shown that large daily doses of riboflavin are not necessary. Improvements can be seen from as large daily dose as 25mg when administered for 3 months.
Research in general shows that administering of B2 vitamin for adults may have positive effect on reducing frequency and duration of migraine episodes without serious side effects. Conclusion: riboflavin seems to be safe and well tolerated solution for migraine symptom prevention in adults.
- Riboflavin is easily destroyed when exposed to light. Milk stored in a glass container and exposed to light loses much of its riboflavin content. Opaque plastic jugs and paper cartons protect the riboflavin in milk. Only small amounts of riboflavin are lost in cooking.
- Out of all of group B vitamins, Riboflavin is probably the most outspoken. It means that you can physically tell if your body has consumed enough Riboflavin as you will notice extra yellow colour of urine if consumption is intense. It is actually the only vitamin that gives you an actual indication of its functioning inside your body! However, due to Riboflavin being water-soluble, your body flushes it out every day, therefore it must be replenished daily.
- To make Vitamin B2 for food supplements or to add it to foods, industrial companies grow special yeasts, fungi, or bacteria that synthesize a lot of Riboflavin.
- Riboflavin is yellow or orange-yellow, so it can be useful as a food coloring. Under a blacklight Riboflavin has ultra-green glow.
- Weight loss increases your need for riboflavin by 60%. More than 20 minutes of cardio exercise 6 days per week increases your need by nearly 60%, too.

Choline
Choline, also known as vitamin B4, is a vital element for functioning of brain and nervous system. It is a component of neurotransmitters that drive communication among nerve cells. It has been found that subjects with sufficient choline intake have better memory and brighter mind. The body obtains majority of choline from diet and only a small amount of it can be produced by the liver.
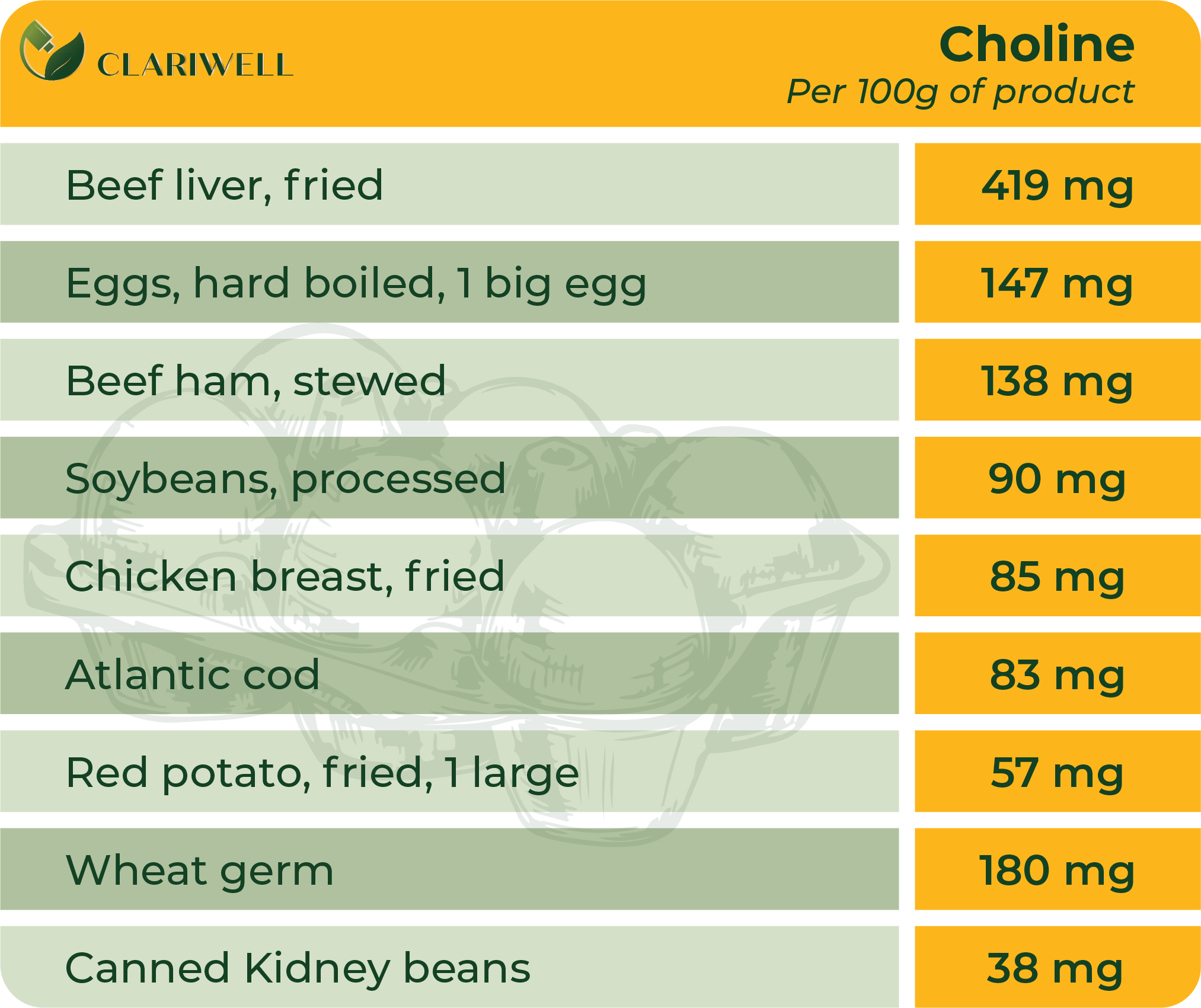
Choline is nutrient similar to the B vitamins. It can be made in the liver. It is also found in foods such as meats, fish, nuts, beans, vegetables, and eggs.
Choline is a source of methyl groups needed for many steps in metabolism. The body needs choline to synthesize phosphatidylcholine and sphingomyelin, two major phospholipids vital for cell membranes. Therefore, all plant and animal cells need choline to preserve their structural integrity.
Choline plays an important part in many processes in the body, including:
- Cell structure: It is needed to make fats that support the structural integrity of cell membranes.
- Cell messaging: It is involved in the production of compounds that act as cell messengers.
- Lipid transport and metabolism: It plays an important role in synthesis of substances that are needed for transporting cholesterol away from the liver. Insufficient levels of choline will cause excessive lipid and cholesterol accumulation in the liver.
- DNA synthesis: Choline and other vitamins, such as B12 and folate, help with a process that’s important for DNA synthesis.
- A healthy nervous system: This nutrient is required to make acetylcholine, an important neurotransmitter. It’s involved in memory, muscle movement, regulating heart rhythm and other vital functions.
Humans can produce choline endogenously in the liver, mostly as phosphatidylcholine, but the amount that the body naturally synthesizes is not sufficient to meet human needs. The most common sources of choline in foods are the fat-soluble phospholipids phosphatidylcholine and sphingomyelin as well as the water-soluble compounds phosphocholine, glycerolphosphocholine, and free choline. When these choline-containing compounds are ingested, pancreatic and mucosal enzymes liberate free choline from about half of the fat-soluble forms and some water-soluble forms.
Citicoline is made up of two molecules: cytidine and choline. There is a view that citicoline multiplies a chemical vital for the brain – phosphatidylcholine. This chemical is important for brain functioning. Citicoline may also increase the amount of other chemicals that ensure communication within the brain.
Citicoline and its hydrolysis products (cytidine and choline) play an important role in phospholipid formation that are involved in building and restoring cellular membranes. It drives also important metabolic functions like nucleic acid protein and acetylcholine formation, where acetylcholine contributes to slowing down heart rate, dilation of peripheral blood vessels and lowering of arterial blood pressure, constriction of bronchi, increasing of peristalsis and secretory activity of the gastrointestinal tract. Acetylcholine contributes to memory improvement and counteracts adrenaline.
Choline deficiency can cause muscle damage, liver damage, and nonalcoholic fatty liver disease (NAFLD or hepatosteatosis). Choline deficiency in healthy, nonpregnant individuals is very rare, possibly because of the contribution of choline that the body synthesizes endogenously.
Although some people believe that vegetarians and vegans may be at risk of choline deficiencies, there is only mixed evidence to support this.
In fact, some of the foods with the highest choline content include soybeans, potatoes, and mushrooms. Eating a nutritious diet that focuses on whole foods should be enough to prevent deficiency.
Adults who are not found or established to be deficient in choline are normally required required 550 mg for men, 425 mg for women of choline per day.
Choline is not known to have any clinically relevant interactions with medications.
Stroke is a devastating neurological disorder and third most common cause of death. Usually stroke causes severe disability, high stroke recurrence risk and other unwanted outcomes. Lack or reduction of blood supply after the ischemic stroke causes internal deviation in functions of organs and systems that lead to damage of the nerve cells.
Underlying causes of neuron death both during ageing and progressing loss of neuron structure and functions both acute and chronic are one and the same. These are excessive accumulation of calcium ions and free radicals in the cell, oxidative stress (it appears if too many free radicals are created in the body that harm health and gradually speed up ageing), mitochondrial dysfunction and metabolic disorders that cause acidosis (acidosis reduces the contractility of heart muscle, causes vessel spasms, deteriorates oxygen supply to tissue. Acidosis also leads to breathing rhythm and consciousness disorders, deteriorates blood supply to the brain and kidneys). As a result, cellular signalling mechanisms that include interaction of thousands of diverse molecules through regulating processes from the membrane to the nucleus and back, are completely inhibited. Meanwhile, a cell that died can neither receive nor transmit nor store information, hence human cognitive (mental) functions undergo neurologic deficit.
Cytidine-5′-diphosphocholine (citicoline or CDP-choline), an intermediate in the biosynthesis of phosphatidylcholine, has shown beneficial effects in a number of CNS injury models including cerebral ischemia. Citicoline is composed of two molecules: cytidine and choline. Cytidine and choline separately pass through the BBB, enter brain cells, and act as substrates for intracellular synthesis of CDP-choline.
Citicoline may:
- decrease release of free fatty acids (excessive amounts of free fatty acids reduce insulin sensitivity or cause insulin resistance in tissue (in liver, heart, muscles and adipose tissue));
- restore mitochondrial adenosine triphosphate (ATF) (a nucleotide with very large impact on metabolism of living organisms and universal energy source for biochemical processes taking place in organisms);
- can be efficiently used in the brain cells for membrane lipid synthesis, where not only it increases phospholipid synthesis but also inhibits degradation of phospholipids;
- reduce or prevent impact of ischemia and/or hypoxia;
- reduce and restrict damage of neuron membranes, restore sensitivity and function of intracellular regulation enzymes and limit oedema;
- promote improvement of concentration, learning and memory performance.
Not only citicoline promotes synthesis of nucleic acid, protein, acetylcholine and other neurotransmitters (biologically active substances that are synthesized in a neuron and is discharged in a synapse; it binds to receptors of other cell and transmits nerve impulse from the synapse to cell), but also reduces formation of free radicals, confirming a view that citicoline at the same time inhibits various steps of ischemic cascades by safeguarding the injured tissues from early or delayed mechanisms that are related to ischemic brain damage. It must be mentioned that citicoline may promote recovery by contributing to synaptic growth and increase neuroplasticity, at the same time reducing neurological deficit and improving behaviour, ability to learn and memory function.
- Not all choline sources are made equally and as much as 50% of the choline we eat may be degraded by bacteria in the gut.
- Choline is not strictly a vitamin, but is an essential dietary amine. It is, however, known in the literature as vitamin B4.
- Choline hydroxide is known as choline base. It is hygroscopic and thus often encountered as a colorless viscous hydrated syrup that smells of trimethylamine (TMA). Aqueous solutions of choline are stable, but the compound slowly breaks down to ethylene glycol, polyethylene glycols, and TMA
- In 1849, Adolph Strecker was the first to isolate choline from pig bile. In 1852, L. Babo and M. Hirschbrunn extracted choline from white mustard seeds and named it sinkaline. In 1862, Strecker repeated his experiment with pig and ox bile, calling the substance choline for the first time after the Greek word for bile, chole, and identifying it with the chemical formula C5H13NO. In 1850, Theodore Nicolas Gobley extracted from the brains and roe of carps a substance he named lecithin after the Greek word for egg yolk, lekithos, showing in 1874 that it was a mixture of phosphatidylcholines.
- In the early 1930s, Charles Best and colleagues noted that fatty liver in rats on a special diet and diabetic dogs could be prevented by feeding them lecithin, proving in 1932 that choline in lecithin was solely responsible for this preventive effect.

Vitamin B9 or folic acid
A water-soluble vitamin necessary for human immune system, cardiovascular and haematopoietic systems. Human body is not able to synthesize folic acid therefore it relies on dietary uptake. Supplementing with this vitamin lowers plasma concentration of homocysteine which in turn reduces the risk of cardiovascular disease.
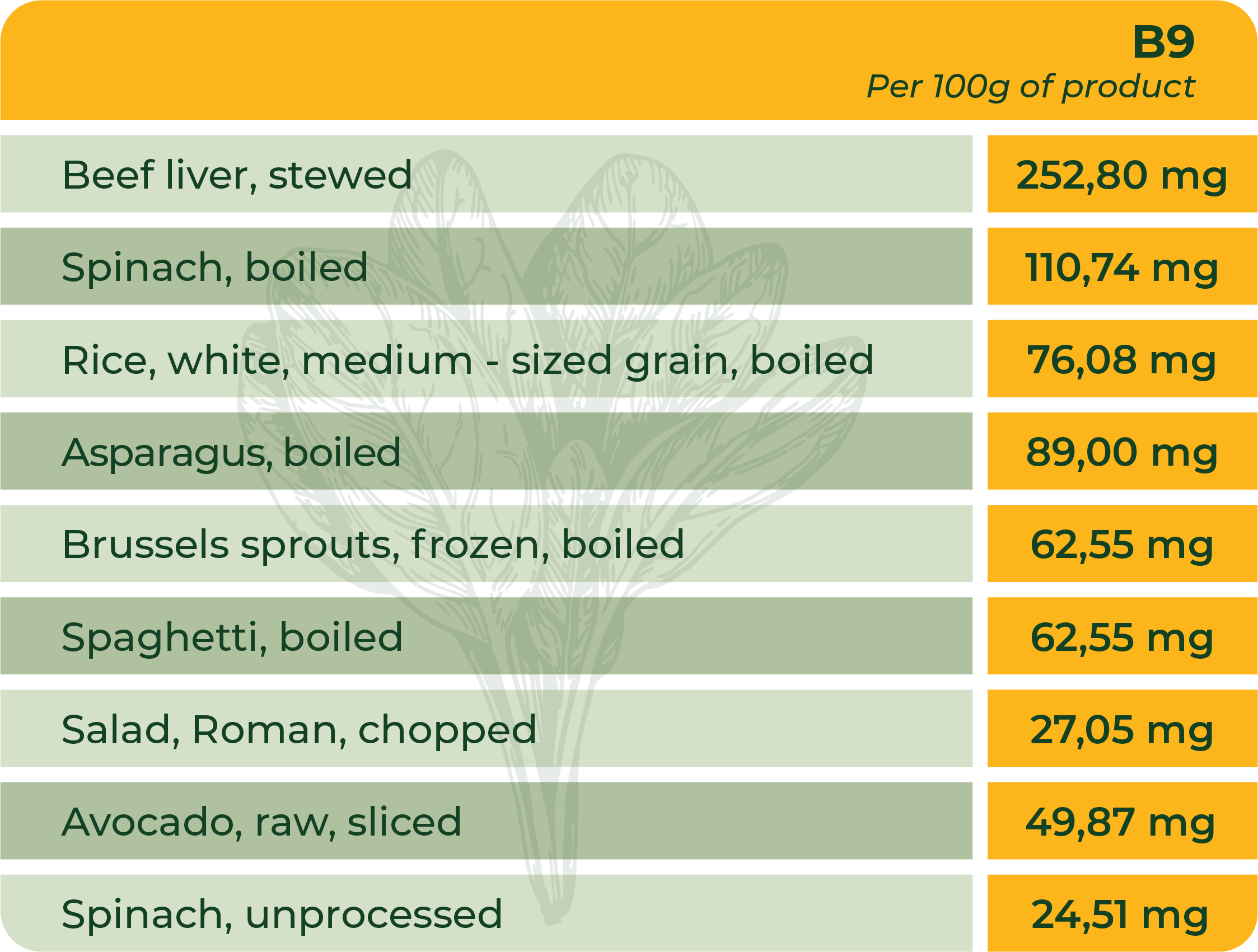
Vitamin B9, also called folate or folic acid, is one of 8 B vitamins. All B vitamins help the body convert food (carbohydrates) into fuel (glucose), which is used to produce energy. These B vitamins, often referred to as B-complex vitamins, also help the body use fats and protein. B-complex vitamins are needed for a healthy liver, and healthy skin, hair, and eyes. They also help the nervous system function properly. Folic acid is the synthetic form of B9, found in supplements and fortified foods, while folate occurs naturally in foods.
All the B vitamins are water-soluble, meaning the body does not store them except for B12 which is stored in liver and used whenever required. Folic acid is crucial for proper brain function and plays an important role in mental and emotional health. It aids in the production of DNA and RNA, the body's genetic material, and is especially important when cells and tissues are growing rapidly, such as in infancy, adolescence, and pregnancy.
One of the most important folate-dependent reactions is the conversion of homocysteine to methionine in the synthesis of S-adenosyl-methionine, an important methyl donor. Another folate-dependent reaction, the methylation of deoxyuridylate to thymidylate in the formation of DNA, is required for proper cell division. An impairment of this reaction initiates a process that can lead to megaloblastic anemia, one of the hallmarks of folate deficiency.
Isolated folate deficiency is uncommon; folate deficiency usually coexists with other nutrient deficiencies because of its strong association with poor diet, alcoholism, and malabsorptive disorders. Megaloblastic anemia, which is characterized by large, abnormally nucleated erythrocytes, is the primary clinical sign of folate or vitamin B12 deficiency. Its symptoms include weakness, fatigue, difficulty concentrating, irritability, headache, heart palpitations, and shortness of breath.
Folate deficiency can also produce soreness in and shallow ulcerations on the tongue and oral mucosa; changes in skin, hair, or fingernail pigmentation; gastrointestinal symptoms; and elevated blood concentrations of homocysteine.
Folate deficiency is rare, but some individuals might have marginal folate status. People with alcohol use disorder frequently have poor-quality diets that contain insufficient amounts of folate. Moreover, alcohol interferes with folate absorption and hepatic uptake, accelerates folate breakdown, and increases its renal excretion
Adults who are not found or established to be deficient in Vitamin B9 are normally required 400 mg (600 mg for pregnant women) of Vitamin B9 per day.
Folate supplements can interact with several medications. A few examples are provided below. Individuals taking these medications on a regular basis should discuss their folate intakes with their healthcare providers.
Methotrexate
Methotrexate (Rheumatrex®, Trexall®), used to treat cancer and autoimmune diseases, is a folate antagonist. Patients taking methotrexate for cancer should consult their oncologist before taking folate supplements because the supplements could interfere with methotrexate’s anticancer effects. However, folate supplements might reduce the gastrointestinal side effects of low-dose methotrexate taken for rheumatoid arthritis or psoriasis.
Antiepileptic medications
Antiepileptic medications, such as phenytoin (Dilantin®), carbamazepine (Carbatrol®, Equetro®, Epitol®), and valproate (Depacon®), are used to treat epilepsy, psychiatric diseases, and other medical conditions. These medications can reduce serum folate levels. Furthermore, folate supplements might reduce serum levels of these medications, so patients taking antiepileptic drugs should check with their healthcare provider before taking folate supplements.
Sulfasalazine
Sulfasalazine (Azulfidine®) is used primarily to treat ulcerative colitis. It inhibits the intestinal absorption of folate and can cause folate deficiency. Patients taking sulfasalazine should ask their healthcare provider whether they should increase their dietary folate intake, start taking a folate supplement, or both.
An elevated homocysteine level has been associated with an increased risk of cardiovascular disease. Folate and other B vitamins are involved in homocysteine metabolism, and researchers have hypothesized that these micronutrients reduce cardiovascular disease risk by lowering homocysteine levels.
Folic acid (and vitamin B12) supplements lower homocysteine levels. However, these supplements do not actually decrease the risk of cardiovascular disease, although they appear to provide protection from stroke.
- Folate and its role in human biochemical functioning was first identified by researcher Lucy Wills in 1931. She found that the nutrient was needed to prevent anemia during pregnancy.
- Folic acid is so important to human health, it is included in many types of foods, especially breakfast cereal. The process to add a vitamin to other foods is called fortification. So, a cereal that has added vitamins is called fortified.
- Folic acid is named from a latin word (folium) which means leaf. This comes from the fact that leafy vegetables are very rich in folic acid.
- Lack of folic acid can also cause a decrease in the amount of red blood cells in the body. This condition is called anemia. The type of anemia caused by folic acid deficiency is called a macrocytic anemia. Macrocytic means "large cells." So, lack of folic acid causes low levels of red blood cells, and the individual red blood cells are really large.
- Folic acid is actually better absorbed by the body than natural folate, almost twice as efficiently.

Vitamin B6
Vitamin B6, also known as pyridoxine, participates in the metabolism of amino acids and fats. Lack of this vitamin causes anaemia, weakness, depression or nervousness, as well as skin inflammation. Vitamin B6 contributes to the formation of red blood cells and haemoglobin.
Vitamin B6 (pyridoxine) was discovered in 1934. It is a water-soluble substance that transforms into the most important coenzymes in the body. Vitamin B6 in the form of a coenzyme fulfils various functions in the body and is extremely versatile, involved in more than 100 enzyme reactions, mainly related to protein metabolism.
Vitamin B6 has three naturally occurring forms: pyridoxine, pyridoxal, and pyridoxamine, all of which transform into their active forms in the body, namely, coenzyme pyridoxal 5-phosphate (PLP or P5P). PLP mainly serves as a coenzyme in the metabolism of amino acids, proteins, carbohydrates and lipids, in addition to the synthesis of neurotransmitters (biologically active substances that are synthesised in the neuron and released in the synapse; when they bind to the receptors of another cell, they transmit the nerve impulse from the synapse to the cell). It is also involved in glycogenolysis and gluconeogenesis.1
Pyridoxine, pyridoxamine, and pyridoxal absorb fast from food and oral drugs and dietary supplements into the mucosal cells of the small intestine, whereas their phosphorylated analogues are first dephosphorylated and then absorbed.
Vitamin B6 has a significant and selectively modulating effect on central serotonin and GABA production2. GABA is a chemical found in the brain and an inhibitory neurotransmitter. Read more about GABA here. It helps to calm the nervous system by blocking certain impulses between nerve cells, slowing down the activity of the brain, thus it has a calming effect that can help reduce stress, anxiety and fear.
Biochemically, in partial vitamin B6 deficiency, some enzymes may be affected more than others, leading to the greater attenuation of certain neurotransmitters and thus disrupting the balance between different neurotransmitter levels.3 Accordingly, causing neurological disorders such as cognitive impairment, convulsive seizures, depression and even premature neuronal ageing (CNS effects).
So, the most important function of vitamin B6 is that it acts as a coenzyme in the synthesis of neurotransmitters necessary for synaptic transmission (for example, dopamine, serotonin, GABA) and performs a neuroprotective role based on its importance in the glutamatergic system.
Vitamin B6 deficiency can be clinically observed as seborrheic dermatitis, microcytic anaemia, tooth decay, glossitis, epileptiform seizures, peripheral neuropathy, electroencephalographic abnormalities, depression, confusion, and weakened immune function.1
Vitamin B6 deficiency is relatively rare, but some people may have low levels of vitamin B6.
People who may be deficient in vitamin B6:
People with impaired kidney function, including those with chronic kidney failure, those receiving maintenance kidney dialysis, those who have had a kidney transplant, often have low levels of vitamin B6.
People with rheumatoid arthritis often have low levels of vitamin B6 in their blood, and these levels tend to decrease as the disease progresses. This low level of vitamin B6 is associated with the inflammation caused by the disease. Although the additional intake of vitamin B6 can normalise blood levels of vitamin B6 in patients with rheumatoid arthritis, it does not, however, suppress the production of inflammatory cytokines and it does not reduce the levels of inflammatory markers, either.
Patients with celiac disease, Crohn's disease, ulcerative colitis, inflammatory bowel disease, and other malabsorption autoimmune disorders typically have low levels of vitamin B6.
People who are dependent on alcohol tend to have very low vitamin B6 concentration levels in the plasma. Alcohol produces acetaldehyde, which reduces net B6 production in cells and competes with pyridoxal 5-phosphate for protein binding. As a result, pyridoxal 5-phosphate may make cells more susceptible to hydrolysis by membrane-bound phosphatase. People with alcohol addiction would be advised to take vitamin B6 supplements regularly.
Adults with no known or confirmed vitamin B6 deficiency normally need 1.3 mg of vitamin B6 per day (pregnant women 2 mg).
High intakes of vitamin B6 from food sources have not been reported to cause adverse effects; however, the long-term use of 1-6 g of oral pyridoxine per day for 12-40 months may cause severe and progressive sensory neuropathy. Degeneration of peripheral nerve fibres and their myelin, as well as spinal canals, causes the bilateral loss of peripheral sensation or hyperaesthesia, accompanied by pain in the extremities, ataxia (impaired movement coordination and balance), and loss of balance. The condition gradually regresses after stopping the use of additional vitamin B6 until normal activity is restored.1 Higher doses may cause testicular atrophy and reduced sperm motility.
Drug interactions
Vitamin B6 can interact with certain medications and several types of medications can negatively affect vitamin B6 levels. Let's cite some examples. Individuals who regularly take these and other medications should discuss their vitamin B6 use with their health care providers.
Cycloserine (Seromycin®) is a broad-spectrum antibiotic used to treat tuberculosis. In combination with pyridoxal phosphate, cycloserine increases the urinary excretion of pyridoxine. Urinary excretion of pyridoxine may exacerbate the convulsions and neurotoxicity associated with cycloserine. Supplemental pyridoxine intake may help prevent these adverse consequences.
Some antiepileptic drugs, including valproic acid (Depakene®, Stavzor®), carbamazepine (Carbatrol®, Epitol® and others), and phenytoin (Dilantin®) increase vitamin B6 catabolism (a set of metabolic processes that break down molecules into smaller units that are oxidised to release energy) rate, resulting in decreased B6 concentrations and the development of hyperhomocysteinemia. High homocysteine levels in antiepileptic drug users can increase the risk of epileptic seizures, including stroke, and reduce the ability to control seizures. In addition, patients typically take antiepileptic drugs for years, increasing the risk of chronic vascular toxicity.
Theophylline (Aquaphyllin®, Elixophyllin®, Theolair®, Truxophyllin®, etc.) can prevent or treat shortness of breath, wheezing, and other breathing problems caused by asthma, chronic bronchitis, emphysema, and other lung diseases. Patients treated with theophylline often have low plasma concentrations of vitamin B6, which may contribute to theophylline-related neurological and central nervous system side effects, including seizures.
In the most recent studies, researchers have looked for a link between mood disorders such as depression and anxiety, stress, and vitamin B6 use. For example, an eight-week phase IV randomised controlled trial found that a combination of magnesium and vitamin B6 was able to provide increased physical activity in daily life and a significant reduction in stress in healthy people with severe stress and anxiety and low magnesium levels.1
Taking the results of various studies into account, it can be concluded that vitamin B6 actively helps to reduce the symptoms characteristic of depression and anxiety, making this vitamin an important addition to everyday life. Another important consideration in favour of vitamin B6 is that while benzodiazepines (such as diazepam, phenazepam, etc.) are effective in treating anxiety and similar conditions, they also have a number of side effects, including but not limited to addiction, rebound anxiety, memory disorders and withdrawal syndrome.

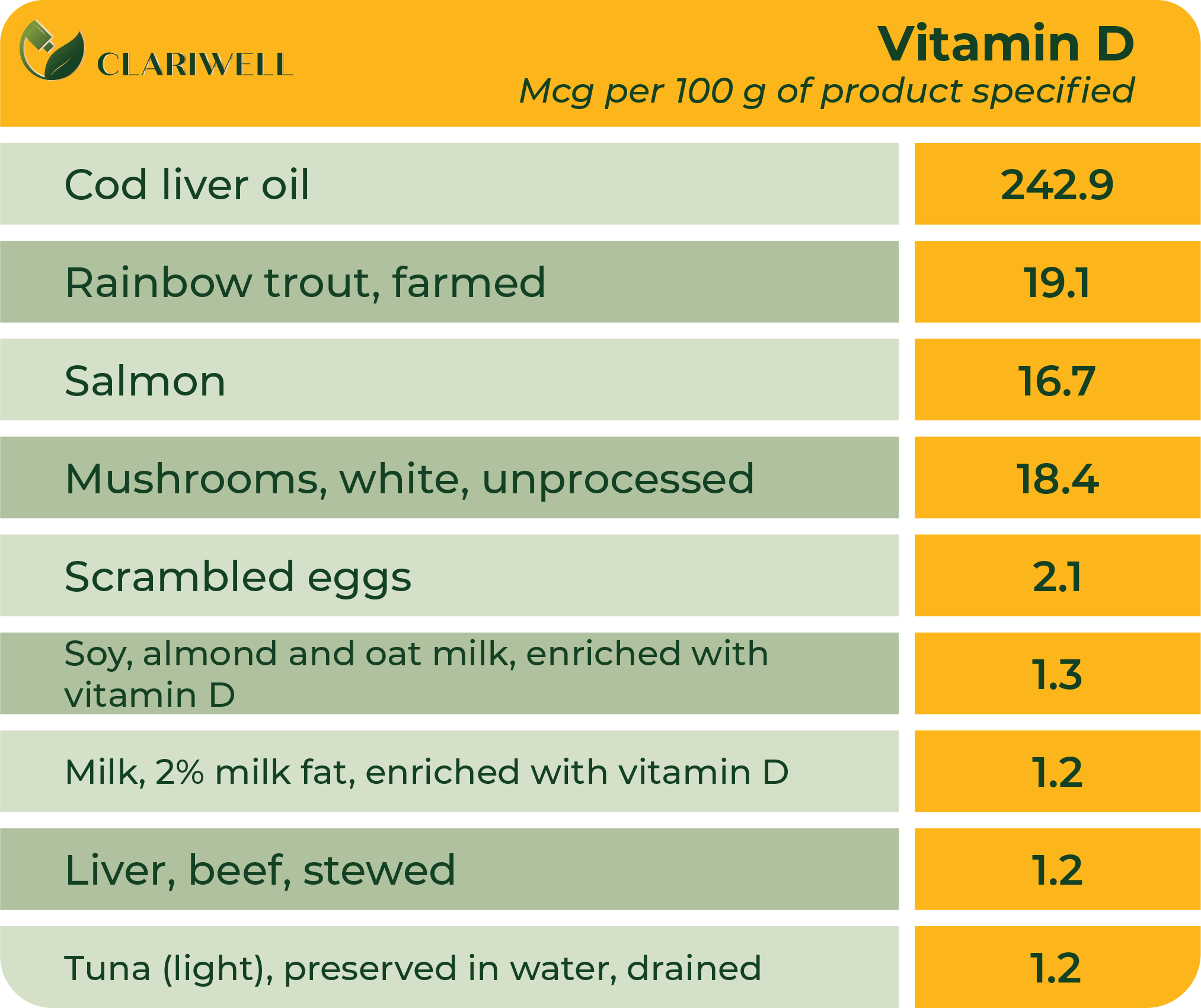
Vitamin D
Vitamin D is a prohormone (hormone precursor) in the group of fat-soluble vitamins. There are five types of vitamin D, ranging from D1 to D5, with two forms being the most common: Vitamin D3 or cholecalciferol and vitamin D2 or ergocalciferol.
Vitamin D helps regulate the amount of calcium and phosphate in the body and is necessary to maintain healthy bones, teeth and muscles. Studies have concluded that vitamin D deficiency is associated with depression and neurocognitive dysfunction, several malignant tumours, and an overall increase in mortality. New studies prove the essential role of vitamin D in maintaining and regulating optimal sleep, as well as the interrelationship between vitamin D concentration, sleep duration and bone metabolism. Vitamin D can modulate innate and adaptive immune responses. Deficiency of vitamin D is associated with increased autoimmunity as well as increased susceptibility to infections.
Vitamin D is a prohormone belonging to the group of fat-soluble vitamins; it is synthesised in the body when the sun's ultraviolet B (UVB) radiation interacts with a precursor molecule, 7-dehydrocholesterol (7-DHC), in the skin (although in healthy people, the internal production of vitamin D is estimated to account for 90% of the total, a small amount of vitamin D is also received from the diet and additional supplements). Vitamin D is then transported in the blood (bound to vitamin D-binding protein) to the liver, where it is hydroxylated to 25-hydroxyvitamin D (25-(OH)D). 25-(OH)D is further converted to the metabolically active form 1α, 25-dihydroxyvitamin D (1α, 25-(OH)2D), mainly in the kidneys.Vitamin D regulates the amount and absorption of calcium ions and phosphates in the small intestine, ensures the formation of bones and teeth, and also helps to strengthen the immune system.
So, for vitamin D to be activated, two metabolic transformations are required - first in the liver - hydrolysis at position 25 (25(OH)D) and then in the kidneys - 1-α-hydrolysis, after which active vitamin D is able to bind to vitamin D receptors to participate in gene transcription and regulated ion (Ca/P) homeostasis.
If we look at the most common forms of vitamin D, D2 (ergocalciferol or calciferol) and D3 (cholecalciferol), it is known that ergocalciferol is mainly obtained from plant sources, formed by UVB radiation in the cell membranes of plants and fungi.
In addition, vitamin D2 is a synthetic molecule that is used to improve food products - added to bread, cereals and dairy products, as well as used in food supplements. Vitamin D3, on the other hand, is obtained from “live” sources, such as fish oil, animal liver and egg yolks. Vitamin D3 is also formed in the skin from provitamin D3 (7-DHC).
Vitamin D deficiency is considered a risk factor for sleep because studies have observed a correlation between vitamin D and sleep duration. Studies of sleep have shown that lower levels of vitamin D are associated with shorter sleep duration in people of all ages. .
An important function of vitamin D is to activate T leukocytes, the cells that actually detect and destroy foreign microorganisms such as viruses. This is why all white blood cells (leukocytes) have vitamin D receptors on their surfaces. Vitamin D can modulate the innate and adaptive immune responses. Deficiency of it is associated with increased autoimmunity as well as increased susceptibility to infections. As immune cells in autoimmune diseases are responsive to vitamin D, it has a beneficial effect in controlling these diseases.
Vitamin D deficiency can occur for various reasons:
- 1. Your eating habits do not include products that are rich in vitamin D; therefore, you do not get enough vitamin D from food;
- 2. Your body does not absorb enough vitamin D from food (malabsorption);
- 3. You spend little time in sunlight or live in a country with little of it, so the body does not receive enough sunlight;
- 4. Your liver or kidneys cannot convert vitamin D into its active form;
- 5. You are taking medicines that prevent your body from converting or absorbing vitamin D.
Vitamin D deficiency can cause a decrease in bone density, which can contribute to osteoporosis and bone fractures. Individuals with vitamin D deficiency have been observed to have improper and restless sleep, as well as other sleep disturbances.
A severe lack of vitamin D can also cause other diseases. It can cause rickets in children. Rickets is a rare disease that causes the bones to become soft and bend. In adults, severe vitamin D deficiency causes osteomalacia. Osteomalacia causes weak bones, bone pain, and muscle weakness.
Researchers are studying vitamin D for its possible connection to several health conditions, including diabetes, high blood pressure, cancer and autoimmune diseases such as multiple sclerosis.
There are some foods that naturally contain vitamin D: fatty fish (such as salmon, tuna, and mackerel), beef liver, cheese, mushrooms, and egg yolks.
Vitamin D can also be obtained from enriched food products. You can check food labels to see if a food contains vitamin D. Food products that are often supplemented with vitamin D include: milk, breakfast cereals and orange juice.
For adults without vitamin D deficiency, the recommended daily dose of vitamin D is 15 mcg or 600 IU, after the age of 70: 20 mcg or 800 IU.
Excessive amounts of vitamin D are toxic. Because vitamin D increases gastrointestinal calcium absorption, vitamin D toxicity results in express hypercalcemia, hypercalciuria, and high serum 25(OH) levels. Hypercalcemia, in turn, can cause nausea, vomiting, muscle weakness, neuropsychiatric disorders, pain, loss of appetite, dehydration, polyuria, excessive thirst, and kidney stones.
In extreme cases, vitamin D toxicity leads to kidney failure, soft tissue calcification throughout the body (including coronary vessels and heart valves), cardiac arrhythmias, and even death.
When taking additional vitamin D, it can interact with several types of medications. Individuals taking these and other medications regularly should discuss vitamin D use and dosage with their healthcare professional.
Orlistat
The weight-loss drug Orlistat (Xenical® and alli®) in combination with a low-fat diet can reduce vitamin D absorption from food and food supplements, thereby reducing 25(OH)D levels.
Statins
Statin drugs reduce cholesterol synthesis. Because endogenous vitamin D is derived from cholesterol, statins can also reduce vitamin D synthesis. In addition, high intakes of vitamin D, especially from food supplements, may reduce the effects of atorvastatin (Lipitor®), lovastatin (Altoprev® and Mevacor®), and simvastatin (FloLipid™ and Zocor®) because these statins and vitamin D compete with each other and the metabolising enzyme itself.
Steroids
Corticosteroid medications are often prescribed to reduce inflammation: budesonide, prednisolone, prednisone, dexamethasone, hydrocortisone, and methylprednisolone (such as Deltasone®, Rayos®, and Sterapred®). These drugs can reduce calcium absorption and interfere with vitamin D metabolism.
Diuretics of the thiazide group
Thiazide diuretics of the thiazide group (such as Hygroton®, Lozol®and Microzide®) reduce urinary calcium excretion. The combination of these diuretics with vitamin D supplements (which increase intestinal calcium absorption) can cause hypercalcemia, especially in the elderly and those with impaired renal function or hyperparathyroidism.
Vitamin D is a prohormone belonging to the group of fat-soluble vitamins. Although vitamin D has traditionally been shown to be involved in calcium homeostasis and bone health, recent studies have found a positive relationship between vitamin D and sleep. In particular, human clinical trials show that low vitamin D levels are associated with poor quality of sleep and short sleep duration. Vitamin D receptors have been found in brain regions involved in sleep regulation, and vitamin D appears to be involved in regulating the sleep-wake cycle.
As we know, vitamin D plays an important role in bone homeostasis and low levels of this vitamin are significantly correlated with low bone mineral density (BMD). Sleep is an important factor in bone metabolism and studies have found a relationship between sleep duration and BMD. In several
self-assessment studies it was reported that decreased sleep duration is associated with decreased BMD and cortical bone thickness.
According to the studies, sleeping less than 5-6 hours is associated with lower BMD and a higher risk of osteoporosis in adults. In children, short sleep duration (<8 h) may be associated with bone mass accumulation disorders during periods of particularly rapid growth. Chronic lack of sleep can directly affect bone metabolism. These discoveries suggest that sleep deprivation may be a risk factor for poorer skeletal health through impaired bone metabolism, may impair bone microarchitecture, and reduce BMD.
In summary, persistent vitamin D deficiency can affect sleep duration, while poor sleep increases the risk of bone fractures and osteoporosis due to impaired bone metabolism.
Vitamin D was used unknowingly to treat infections such as tuberculosis before the advent of effective antibiotics. Tuberculosis patients were sent to sanatoriums where treatment included exposure to sunlight, which was thought to directly kill the tuberculosis. Cod liver oil, a rich source of vitamin D, has also been employed as a treatment for tuberculosis as well as for general increased protection from infections.
The beneficial effects of vitamin D on protective immunity are in part due to its effects on the innate immune system It is known that macrophages recognise lipopolysaccharides (known as endotoxins, which are formed when bacteria are killed) through TLR receptors, which trigger an immune cell response. Engagement of TLRs leads to a cascade of events that produce antimicrobial peptides with potent bactericidal activity that disrupt bacterial cell membranes, such as cathelicidin and beta defensin.
With the direct help of vitamin D, our bodies produce more than 200 antimicrobial peptides, the most potent of which is cathelicidin, a natural broad-spectrum antibiotic. This explains the effectiveness of vitamin D therapy in treating all types of acute respiratory viral infections.
In general, vitamin D helps reduce viral replication by inducing defensins and cathelicidins, and minimises the total amount of cytokines (biochemically active intercommunicating protein molecules produced by immune cells to act on other immune cells) that injure the lung mucosa in inflammatory pneumonia, and helps increase anti-inflammatory cytokines.

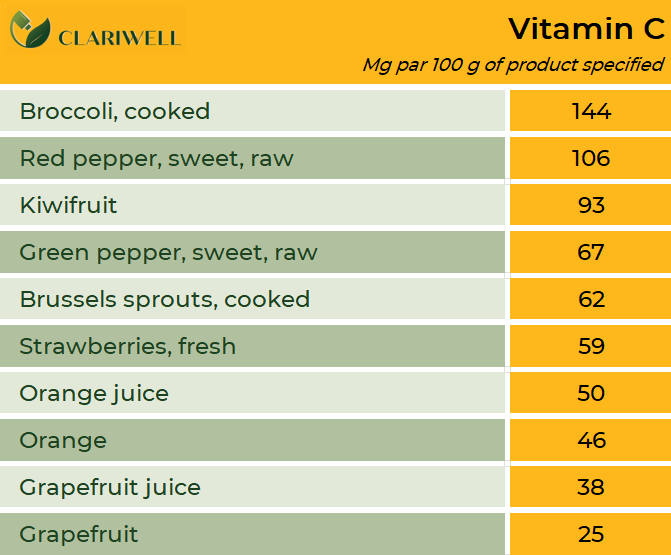
Vitamin C
Vitamin C, or ascorbic acid, is an essential micronutrient for normal metabolic function, essential for tissue growth and repair throughout the body. It is a water-soluble vitamin, but the body does not produce it itself. As an antioxidant, vitamin C fights free radicals in the body, which may help prevent various diseases and promote healthy ageing. Vitamin C acts as a “helping molecule” for several enzymes involved in biosynthesis.
The empirical formula of vitamin C is C6 P8 O6. It is a crystalline powder, white or slightly yellow in colour, practically odourless and with a very sour taste. The melting point is 190 degrees Celsius. The active components of the vitamin are normally destroyed by cooking food, especially in the presence of metals such as copper. Vitamin C may be considered the most unstable of all the water-soluble vitamins, but it can withstand freezing. It is easily soluble in water and methanol and oxidises well, especially in the presence of heavy metal ions (copper, iron, etc.). It gradually darkens in contact with air and light. In the absence of oxygen, it can withstand temperatures of up to 100 °C. Vitamin C is an essential element that must be consumed in the diet because the body cannot synthesise it. Thus, our body has developed an efficient adaptive system to maintain organic reserves of vitamin C and prevent its deficiency in the case of malnutrition. Dietary vitamin C is absorbed in the reduced form of ascorbic acid through intestinal tissues, via the small intestine, by active transport and passive diffusion via SVCT transporters 1 and 2.
Vitamin C does not have to be digested before absorption. Ideally, about 80–90% of vitamin C consumed is absorbed from the intestines. However, the absorption capacity of vitamin C is inversely related to intake; it tends to reach 80–90% efficiency at quite low levels, but these percentages decrease significantly if the daily intake exceeds 1 gram. Given normal intake with food, 70–90% of vitamin C is absorbed at moderate intakes of 30–180 mg/day, but increases to 98% with very low intakes (less than 20 mg). And vice versa, at doses above 1 g/day, absorption falls to less than 50% The whole process is very fast; the body takes up the required amount in about two hours, and within three to four hours the unused part is removed from the bloodstream. It is even faster for people who consume alcohol or smoke cigarettes, and under stressful conditions. Many other substances and conditions can also increase the body’s need for vitamin C: fever, viral diseases, antibiotics, cortisone, aspirin and other painkillers, exposure to toxins (such as petroleum products, carbon monoxide) and heavy metals (such as cadmium, lead, mercury).
In fact, the white blood cell concentration of vitamin C can reach up to 80% of the plasma concentration of vitamin C. However, the body has a limited storage capacity for vitamin C. It is most often maintained in the adrenal glands (about 30 mg), pituitary gland, brain, eyes, ovaries, and testicles. Vitamin C is also found in the liver, spleen, heart, kidneys, lungs, pancreas and muscles, although in smaller amounts. Plasma concentration of vitamin C increases with increasing intake, but only up to a certain limit. Any dose of 500 mg or more is normally removed from the body. Unused vitamin C is removed from the body or first converted to dehydroascorbic acid. This oxidation mainly happens in the liver and also in the kidneys.
Pharmacokinetic experiments demonstrated that plasma vitamin C concentration is tightly controlled by three primary mechanisms: intestinal absorption, tissue transport, and renal reabsorption 100% absorption efficiency is observed with oral intake of vitamin C in doses of up to 200 mg at one time. Once plasma vitamin C concentrations reach saturation, additional vitamin C is largely excreted in the urine.
The first symptoms of vitamin C deficiency in the body are weakness and fatigue, muscle and joint pain, rapid bruising, and rashes in the form of small red-blue spots. Other symptoms include dry skin, swollen and discoloured gums, bleeding gums, wound healing, frequent colds, tooth loss and weight loss.
In 2013, the European Scientific Committee on Food stated that the average vitamin C requirement for a healthy level is 90 mg/day for men and 80 mg/day for women. The ideal amount for most people is around 110 mg/day for men and 95 mg/day for women. According to the group of experts, these levels were sufficient to balance the metabolic losses of vitamin C and to maintain plasma ascorbate concentrations at around 50 µmol/L.
Smokers are recommended to take 35 mg/day more than non-smokers because they are exposed to increased oxidative stress caused by cigarette smoke toxins and generally have lower vitamin C levels in the blood.
It is currently recommended to avoid doses of vitamin C higher than 2 g/day to avoid side effects (bloating and osmotic diarrhoea). It is believed that excessive consumption of ascorbic acid can cause several problems (e.g., birth defects, cancer, atherosclerosis, increased oxidative stress, kidney stones); however, none of these alleged adverse health effects have been confirmed in subsequent studies, and there is no reliable scientific evidence. Although, there is scientific evidence that high levels of vitamin C (up to 10 g/day in adults) are toxic or detrimental to health. Gastrointestinal side effects are usually not serious and normally disappear when high doses of vitamin C are reduced. The most common symptoms of vitamin C overdose are diarrhoea, nausea, abdominal pain and other gastrointestinal problems.
Some medicines can lower vitamin C levels in the body: oral contraceptives, high doses of aspirin. Taking vitamin C, vitamin E, beta-carotene and selenium at the same time can reduce the effectiveness of cholesterol-lowering drugs and niacin. Vitamin C also interacts with aluminium, which is part of most antacids, so a break between their use is necessary. In addition, there is some evidence that ascorbic acid may reduce the effectiveness of some cancer and AIDS drugs.
Vitamin C (ascorbic acid) plays an important role in the normal functioning of the immune system and its use in preventing and/or treating infections has strongly attracted the interest of physicians and investigators for almost a century. It is well known that vitamin C deficiency leads to increased vulnerability to infections.
In the 1970s, Linus Pauling proposed that vitamin C could successfully treat and/or prevent the common cold. The results of further controlled studies have been inconsistent, leading to confusion and controversy, although public interest in the subject remains high.
One study examined placebo-controlled trials of 200 mg of vitamin C per day taken continuously as prophylactic treatment or after the appearance of cold symptoms. Prophylactic vitamin C intake did not generally reduce the risk of common cold. However, in studies involving marathon runners, skiers and soldiers exposed to extreme exercise and/or cold environments, prophylactic vitamin C intake of 250 mg/day to 1 g/day reduced the occurrence of common colds by 50%. In the general population, Prophylactic supplementation with vitamin C reduced the duration of the common cold in both adults by 8% and children by 14%. When taken after the occurrence of cold symptoms, vitamin C had no effect on the duration or severity of colds.
However, vitamin C has generally been shown to regulate the immune system due to its antioxidant properties and its role in the synthesis of collagen, which is needed to stabilise epithelial barriers. Additionally, it impacts phagocytic function and has an immune-stimulatory effect on lymphocyte cells. Vitamin C is highly concentrated in leukocytes and is used rapidly during infection. In fact, it has been defined as a stimulant of leukocyte functions, especially of neutrophil and monocyte movement. High vitamin C levels in neutrophils are necessary to counteract the extremely high levels of oxidative stress, which includes damage to cellular DNA and cell bodies caused by molecules known as reactive oxygen species (ROS), also known as “free radicals”. The antioxidant balance is an important determinant of immune function and immune cells are particularly sensitive to changes in this balance.
Also, vitamin C has good synergy with immune-boosting substances such as beta-glucans. The potent immune-stimulatory effects of beta-glucans are well established, with recent studies showing that some additional bioactive molecules have synergistic effects when combined with glucan. First, several scientific studies have confirmed the beneficial effects of taking glucan in combination with vitamin C. The main reason for the synergistic effect of vitamin C could be the fact that vitamin C stimulates the same type of immune responses as glucan.
Accordingly, we can conclude that vitamin C is an essential antioxidant and plays an important role as a cofactor (helps catalyse biochemical reactions) and modulator of various immune system pathways.
- In the 1940s, Doctor Frederick Klener cured chickenpox, tetanus, mumps, measles and poliomyelitis using vitamin C therapy.
- Vitamin C is excellent for collagen repair. It helps the skin look better and relieves bone pain.
- Scurvy was a disease that most sailors had to deal with. For a long time, nobody knew how to treat this disease. Around 1747, a breakthrough came. A doctor managed to cure 12 sick sailors with citrus fruits. It was the only effective treatment and eventually gave the sailors the nickname “sour”. It originated from sucking on limes during a voyage to prevent illness.
- Vitamin C is necessary for proper fat metabolism. Basically, it allows the body to use fat as fuel. It has also been proven that vitamin C can help reduce appetite.
- Vitamin C, instant coffee and soda can be used to develop black-and-white films.
- Humans, primates and guinea pigs are the only mammals that cannot produce vitamin C in their own bodies.
 Free delivery to Omniva parcels throughout the Baltics for purchases from 20 euros!
Free delivery to Omniva parcels throughout the Baltics for purchases from 20 euros!